hall ticket no. 1601006117 long case medicine
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
MEDICINE FINAL EXAM.HSP
A CASE OF MULTIPLE SKIN LESIONS THAT KEEPS REAPPEARING.,WHAT COULD BE THE CAUSE??
April 24, 2021
A 23 year old lady,Psychologist by Occupation resident of Nalgonda Came to the OPD with chief complaints of Multiple small Painful red color skin eruptions over the upper and lower limbs and back of the trunk since 8 months
History of presenting illness:
Patient was apparently asymptomatic 8 months ago then she developed multiple small red Palpable eruptions on both lower limbs which was not associated with Burning or itching and after 1 week She developed Occasional Burning Over the lesions she consulted a local dermatologist where she was prescribed antihistamines and was asked to avoid oily foods and vitamin C and the lesions didn't subside so she was referred to another Hospital where she was diagnosed with HENOCH SCHONLEIN PURPURA ?
She was asked for CUE, ASO TITRE, ESR, RFT,Serum Bilirubin which was normal and diascopy showed Non blanchable palpable erythamatous Purpura and was prescribed
- Antihistaminics[Tab. TECZINE 5 mg]
- Calosoft lotion
- Halovate lotion
◇After 1 week new purpuric lesion started to develop Over the thighs and she was prescribed the following after Serum Creatinine and Uric acid were Normal
- OMNACORTIL 20mg
- PANTOP 40 Mg
◇After 2 Weeks she has history of travel for 3 days during which she developed
- painful Soles on both the legs and Same medicines were continued
- the next day She presented with increased number of purpuric lesions Over both the legs and they were Spread to hands and back of the trunk associated with pain, itching and Burning Sensation
- history of Joint pains initially in the left wrist later Progressed to left elbow
- She had Pedal edema and Pain in the lower limbs
- abdominal Pain the previous night and no history of fever
The following investigations were done:
⊙Haemogram showed normochromic normocytic Blood Picture with Neutrophilic leucocytosis
and She was prescribed Tab. ZERODOL and Tab. SHELCAL in addition to above medication.
◇After a week She presented with Weight gain of 5kgs in a week and Facial Puffiness. on Examination striae were Seen on legs and thighs and few purpurae located Over thighs, legs and dorsum of Hand(lesions are decreased in number) and Steroid induced Weight gain or Cushing's Syndrome was Suspected to be the Cause.
→ Advised to Consider using immunosuppressants and taper steroids.
→Steroid dose was reduced from 20 mg to 15 mg and Tab. METHOTREXATE 2.5 mg test dose was given and Tab.FOLIC ACID 5mg on a day other than Methotrexate
◇After 10 days She complained abdominal pain which improved by next morning and her Methotrexate dose was increased to 7.5 mg and FUDIC CREAM Was prescribed
◇On follow up after a week She was found to tolerate the dose of Methotrexate Well with reduction in number of new lesions and the above drugs were continued with addition of MOISTUREX Soft cream
◇4 days later improvement was Seen with mild pain on both the soles ( Pain was reduced in intensity) and
- Methotrexate dose was increased to 10 Mg
- folic acid on the day other than Methotrexate
- Tab. ZERODOL P(SOS)
- Tab. MVT
◇ on follow up after a week Improvement was Seen with a Cummulative dose of 30 mg and She Complained of mild itching and Burning Sensation near the groin.
On Examination Single Hyperpigmented plaque noted over Pubic area which aggravated on Using Sanitary Napkins and was prescribed LULIFIN cream
◇4 days later improvement was Seen with Cumulative dose of Methotrexate 50 mg and following drugs were Prescribed
- LIVOGEN on day other than Methotrexate
- Methotrexate12.5 mg
- Tab. SUPRADYNE
- ABZORB Dusting Powder
◇2 Weeks later improvement was seen Cumulative dose of Methotrexate75 mg and the above medications were continued and 1 week later She Complained of Nausea, loss of appetite and Insomnia and she was Prescribed Tab. Amitriptyline 5 mg
◇ 2 weeks later She Showed Painful skin lesions on both palms and Soles with Cumulative dose of Methotrexate 125 mg and She was prescribed
- METHOTREXATE 12.5 mg
- VENUSIA Soft lotion on itchy lesions
- NMFE lotion over stretch marks and all over the body
- Tab. LIVOGEN on day other than Methotrexate
- Tab. SUPRADYNE
◇2 Weeks later She presented with new lesions over Palms associated with itching (Cumulative dose of Methotrexate 150 mg) and Tab. TECZINE 10 mg and Tab. PANTOP-D was prescribed
◇ 20 days later She presented with new lesions Over Palms and soles and between the Web Spaces Since1 week and pain of Soles while walking especially early in the morning and on examination Multiple erythematous pin point Sized Papules noted all over the palms,Web Spaces and both Soles ( Cumulative dose of Methotrexate 170 mg )
- Methotrexate dose reduced to 5 mg Once weekly for 2 Weeks and then 2:5 mg Weekly once for1 week
- MOMATE Cream on alternate days over the lesions
- Liquid PARAFFIN
◇10 days later She complained of appearance of new lesions and was advised to Stop all medications and report to OPD for Skin biopsy and was prescribed Tab.DEFZA 12 mg and Tab. TECZINE 5 mg (for pain)
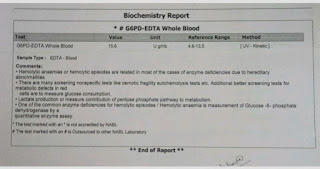
◇2 weeks later, Biopsy was done and Histopathological report showed Neutrophilic Leucocytoclastic Vasculitis and was advised to check G6PD levels and was prescribed Tab. DAPSONE 50mg
*20 days later She presented with Itchy purpura Over both feet
and was prescribed
- Tab.TAXIM-O 100 mg
- Tab. ASCARZIN
- Tab. EVION 400 mg
- Tab. DAPSONE 50 mg
- ATARAX anti itch lotion
◇15 days later She presented with Complaint of new lesions and was advised to get
- Haemogram [ Hb-11.6 g /dl, PCV-33.7 vol% , RBC-3.7 mil/mm³]
- Peripheral Smear [normochromic normocytic RBC with WBC in normal limits]
- D-Dimer [elevated]
- Prothrombin time[14 sec]
- APTT [28 sec]
☆She had no history of hematuria,hematemesis and epistaxis
> Past history:
No History of similar complaints in the past, she is not a k/c/o diabetes mellitus, hypertension, epilepsy, tuberculosis, asthma.
☆ family history:
No similar complaints in the family
☆ personal history:
- mixed diet,
- normal appetite,
- sleep adequate
- bowel and bladder movements- regular
- no addictions and no known drug allergies
☆ general physical examination:
patient is conscious, coherent,cooperative and moderately built and moderately nourished
Vitals:
→ patient is afebrile
→ BP-110/80 mm Hg
→ PR-70 bpm
→ RR-16 Cpm
✓SpO2- 98%
✓GRBS - 122gm/dl
→There was no Pallor, Icterus, Cyanosis, clubbing, Odema, lymphadenopathy.
*on inspection:
red erythematous lesions Over Hands, legs, Palms and Soles including Web Spaces
*CNS examination:
- Higher mental functions-normal
- Cranial nerves- intact
- Sensory system- normal
- Motor system- normal
- Meningeal signs- absent
- Cerebellar signs- absent
*Cvs examination:
Inspection :
No scars sinuses and engorged ve
No visible pulsation
Palpation:
apical impulse : heard in fifth inter coastal spac
Auscultation:
S1 and S2 hear
No murmursd on:e on:sins.
No murmurs heard
*Respiratory system examination:
Inspection of upper respiratory system-
oral cavity- normal
Nose- normal
Pharynx- normal
Lower Respiratory Tract:
Inspection:
trachea: central
Symmetry of chest : symmetrical
Movement: B/L symmetrical expansion of chest respiration
No scars, engorged veins or sinuses.
Palpation:
All inspectory findings are confirmed by palpation.
Trachea: central - confirmed by three finger test.
Assessment of anterior and posterior chest expansion- B/L symmetrical expansion of chest.
No chest wall tenderness
Vocal fremitus- normal
Percussion :
done in sitting position
Resonant
Auscultation:
Vesicular breath sounds heard
Bilateral air entry present
No added sounds
*Abdominal examination:
Inspection:
Shape : elliptical
Quadrants of abdomen moving in accordance with respiration.
Umbilicus- central and inverted
No scars sinuses or engorged veins
Palpation:
No tenderness
No organomegaly
Percussion:
tympanic
Auscultation:
Normal
No organomegaly , no tenderness.
Investigations reports:
PROVISIONAL DIAGNOSIS- HENOCH SCHONLEIN PURPURA ( Leucocytoclastic Vasculitis)
Treatment:
At present patient is using:
- Tab. Dapsone 100mg
- Syrup orofer 5ml
- Tab. Shelcal




























Comments
Post a Comment